- CRRT is indicated to correct metabolic or fluid derangements associated with acute renal failure in hemodynamically unstable patients
- Continuous venovenous hemofiltration (CVVH) is the most common mode used in surgical intensive care units
- The right internal jugular vein is the first choice for CRRT catheter access, followed by the femoral vein and the left jugular vein
- Anticoagulation of the CRRT circuit with citrate has been found to be superior in terms of safety, efficacy, and cost compared to heparin
- Criteria for terminating CRRT: spontaneous urine output > than 400 mL/day, correction of metabolic derangements, no need for clearance, and stabilization of fluid balance
Latest Updates
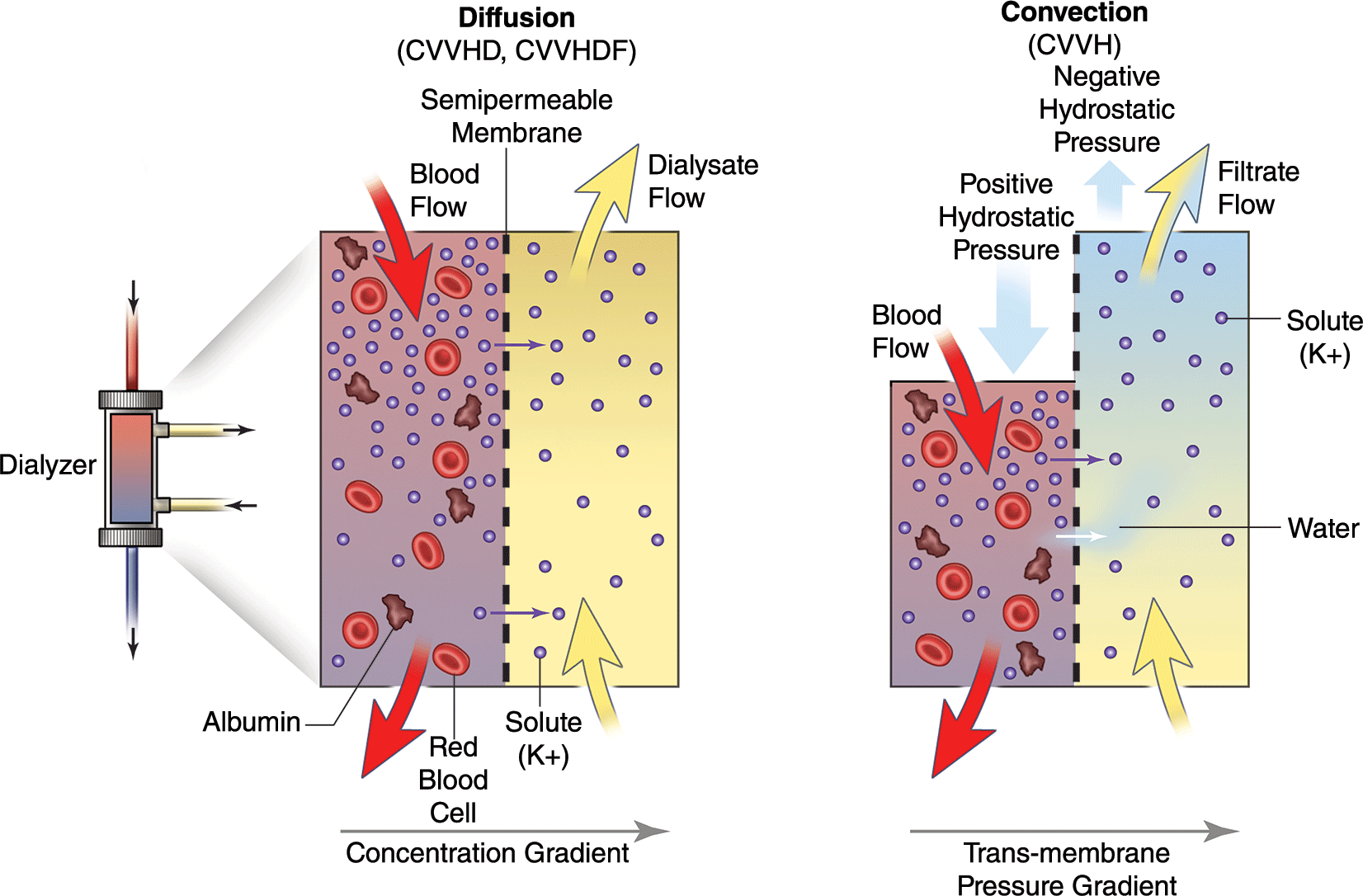
- CRRT is indicated to correct metabolic or fluid derangements associated with acute renal failure in hemodynamically unstable patients
- Continuous venovenous hemofiltration (CVVH) is the most common mode used in surgical intensive care units
- The right internal jugular vein is the first choice for CRRT catheter access, followed by the femoral vein and the left jugular vein
- Anticoagulation of the CRRT circuit with citrate has been found to be superior in terms of safety, efficacy, and cost compared to heparin
- Criteria for terminating CRRT: spontaneous urine output > than 400 mL/day, correction of metabolic derangements, no need for clearance, and stabilization of fluid balance
- National organizations such as the Trauma Quality Improvement Program of the American College of Surgeons have described the importance of palliative care integrated throughout the clinical course.
- Increasing numbers of surgeons are fellowship trained and certified by the American Board of Surgery in Hospice and Palliative Medicine in addition to surgical specialties.
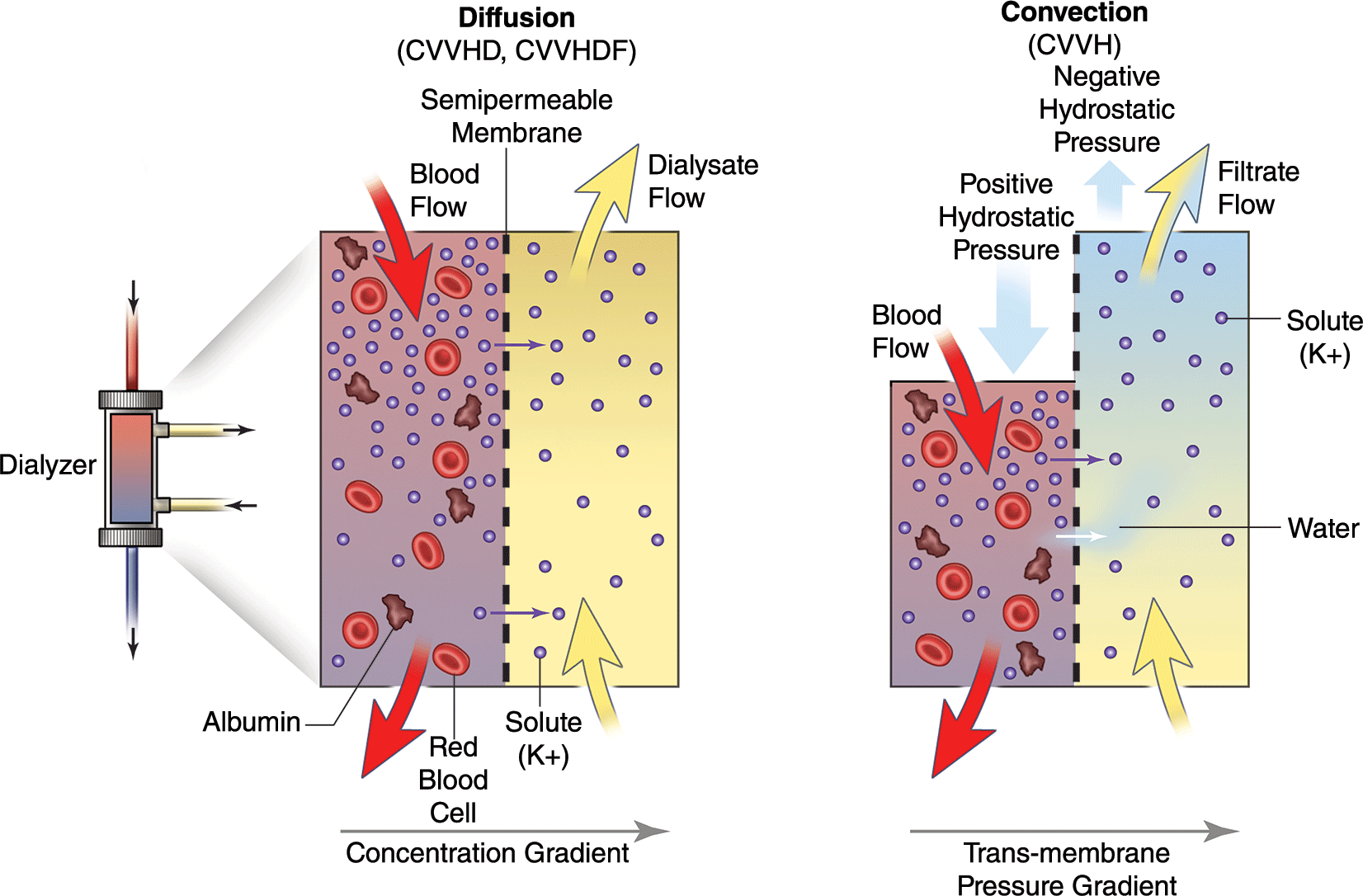
- The importance of accurate prognostication for surgical patients and thoughtful communication of anticipated outcomes of different treatment plans has been recognized through frameworks such as the “Best Case/Worst Case” scenario.1
- Structured descriptions of gaps and opportunities in the field promote future advancement and development of surgical palliative care.
- Studies in surgical and nonsurgical patients demonstrate that palliative care, hospice enrollment, and lower-intensity end-of-life care do not decrease survival.

- Consideration of form and function is paramount in nasal reconstruction and underlying nasal obstructive pathology should be identified prior to reconstruction. It may be prudent to correct at the time of reconstruction.
- There are many options for reconstruction of nasal lining defects, but all have some drawbacks. A familiarity with all techniques is mandatory for the reconstructive surgeon.
- The paramedian forehead flap is the work-horse for major nasal reconstruction and all facial reconstructive surgeons should be facile with its application.
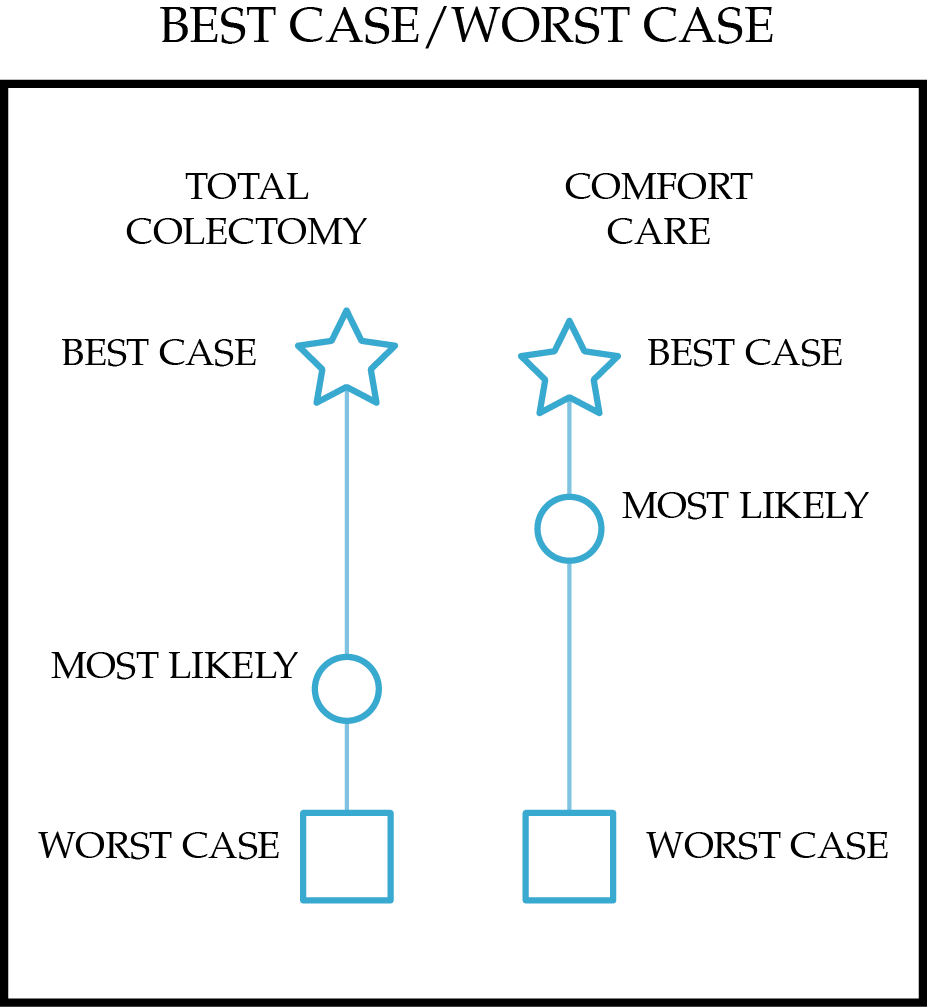
- Recent changes in Clinical Practice Guidelines consider tonsillectomy in recurrent tonsillitis as a treatment option rather than a recommendation
- Novel techniques and surgical tools in tonsillectomy include microdebriders and bipolar cold ablation devices, but more robust evidence is warranted before a recommendation as a standard of care is issued
- More well-designed clinical trials are required to compare different surgical techniques in tonsillectomy
- Periodic fever syndromes associated with recurrent tonsillitis remain a potential “hot topic” for future research
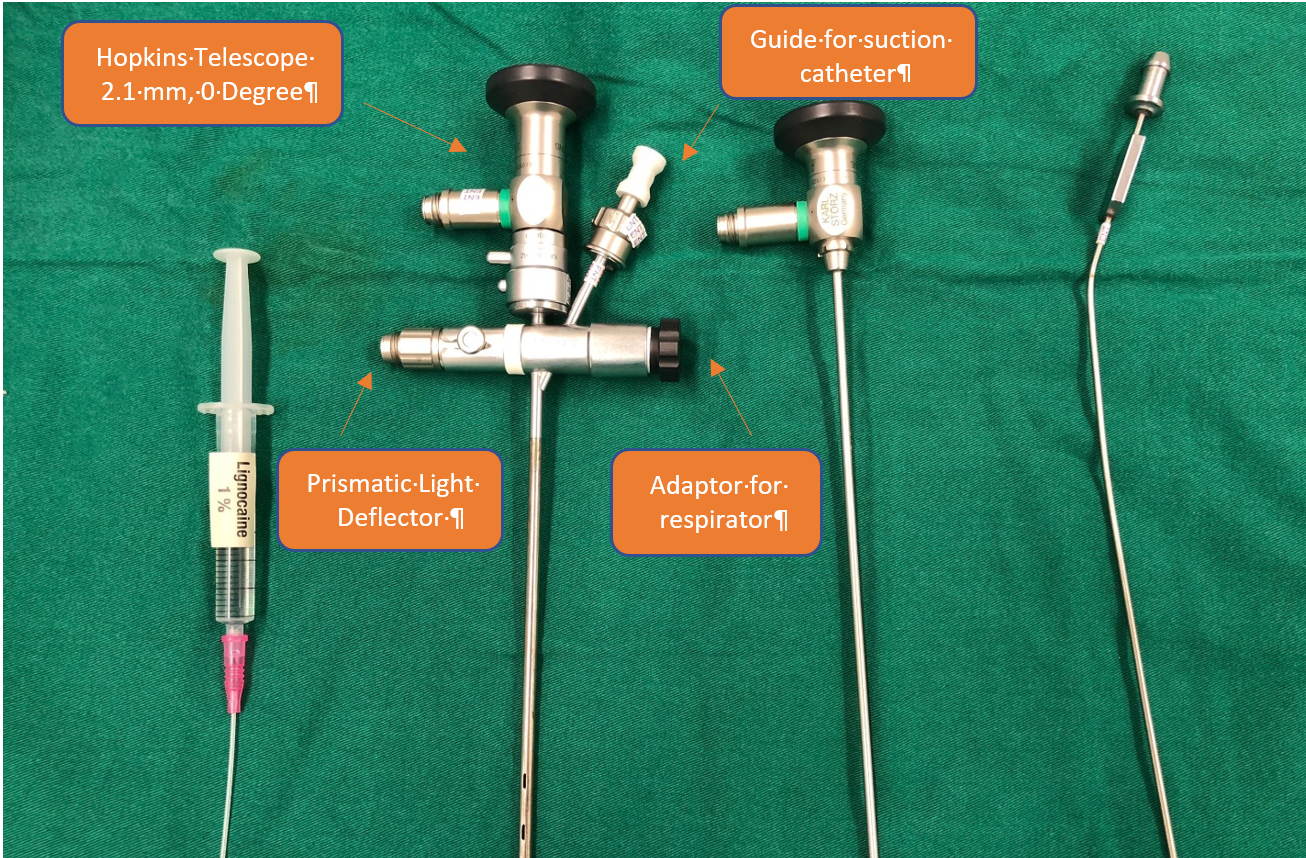
- Technologic advances and development of specialized endoscopic tools (eg airway balloons) has resulted in new era of endoscopic airway surgeries.
- Propranolol use for airway hemangiomas has revolutionized treatment.
- Systemic Bevacizumab (Avastin) has shown promising results in severe Juvenile onset recurrent respiratory papillomatosis(JORRP).
- Haemophilus influenzae B (HIB) vaccine has essentially eliminated HIB-induced epiglottitis.
- Improved airway management of an intubated infant has led to reduced acquired subglottic stenosis.
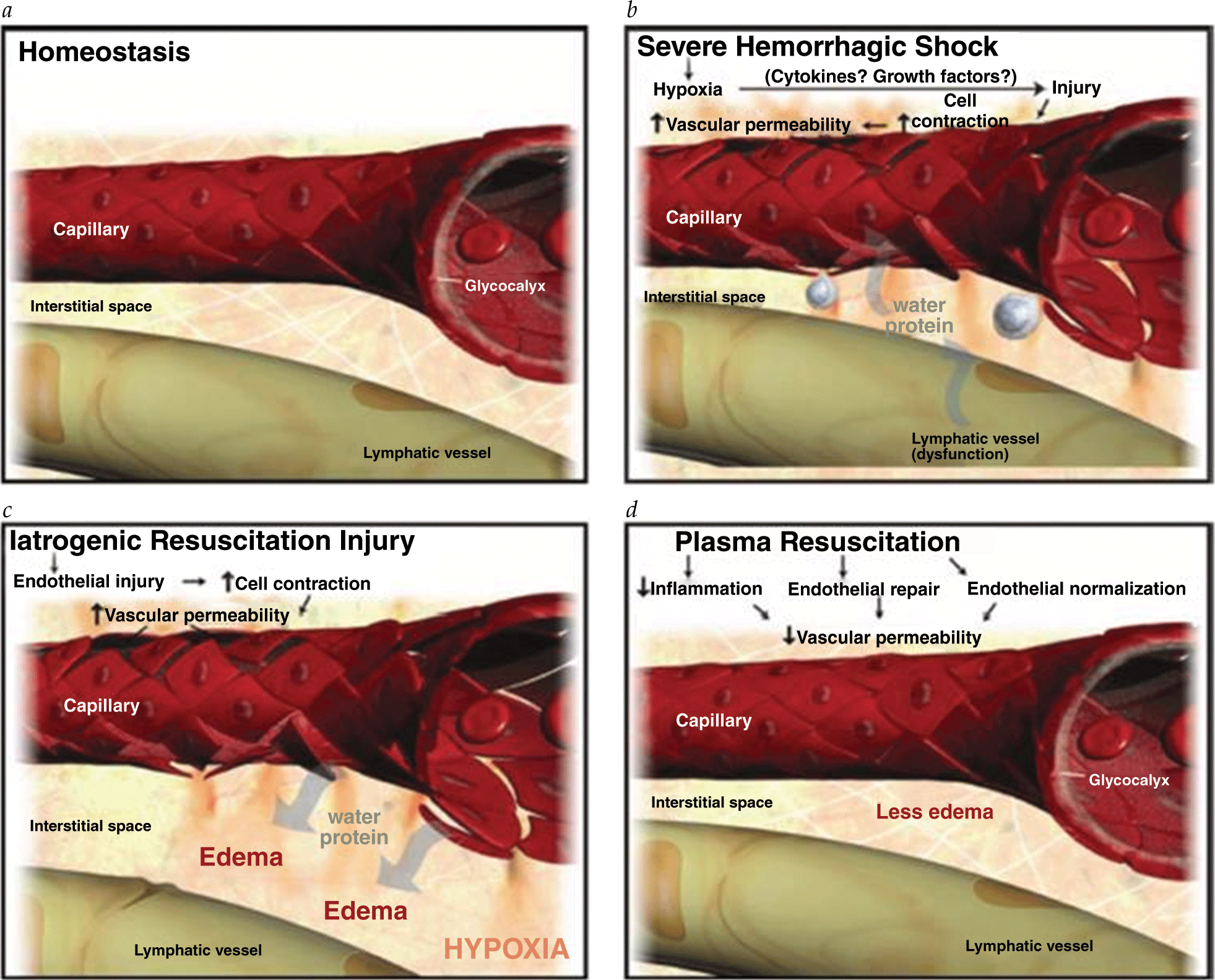
- The Committee on Trauma of the American College of Surgeons (ACS-COT) mandates that high-level trauma centers develop a predefined MTP that can be activated to quickly transfuse rapidly hemorrhaging patients. Early activation of a predefined MTP is associated with more efficient use of blood products (reducing waste) and improved patient outcomes. However, early identification of the bleeding patient remains a challenge.
- Viscoelastic assays such as thromboelastography (TEG) and rotational thromboelastometry (ROTEM) assess the coagulation profile of a whole blood sample. Significantly, different parameters derived from the TEG and ROTEM tracings are related to different components of coagulation, enabling targeted correction of abnormalities.
- Although it seems natural and intuitive to follow the same protocol to treat patients with substantial nontraumatic hemorrhage, there is little scientific evidence to support this practice. Of the few studies investigating optimal blood product ratios of nontraumatic hemorrhage available in the literature, MT was unfortunately defined using the outdated criterion of 10 RBC units or more in 24 hours, which, as we have previously stated, is fraught with survivor bias.
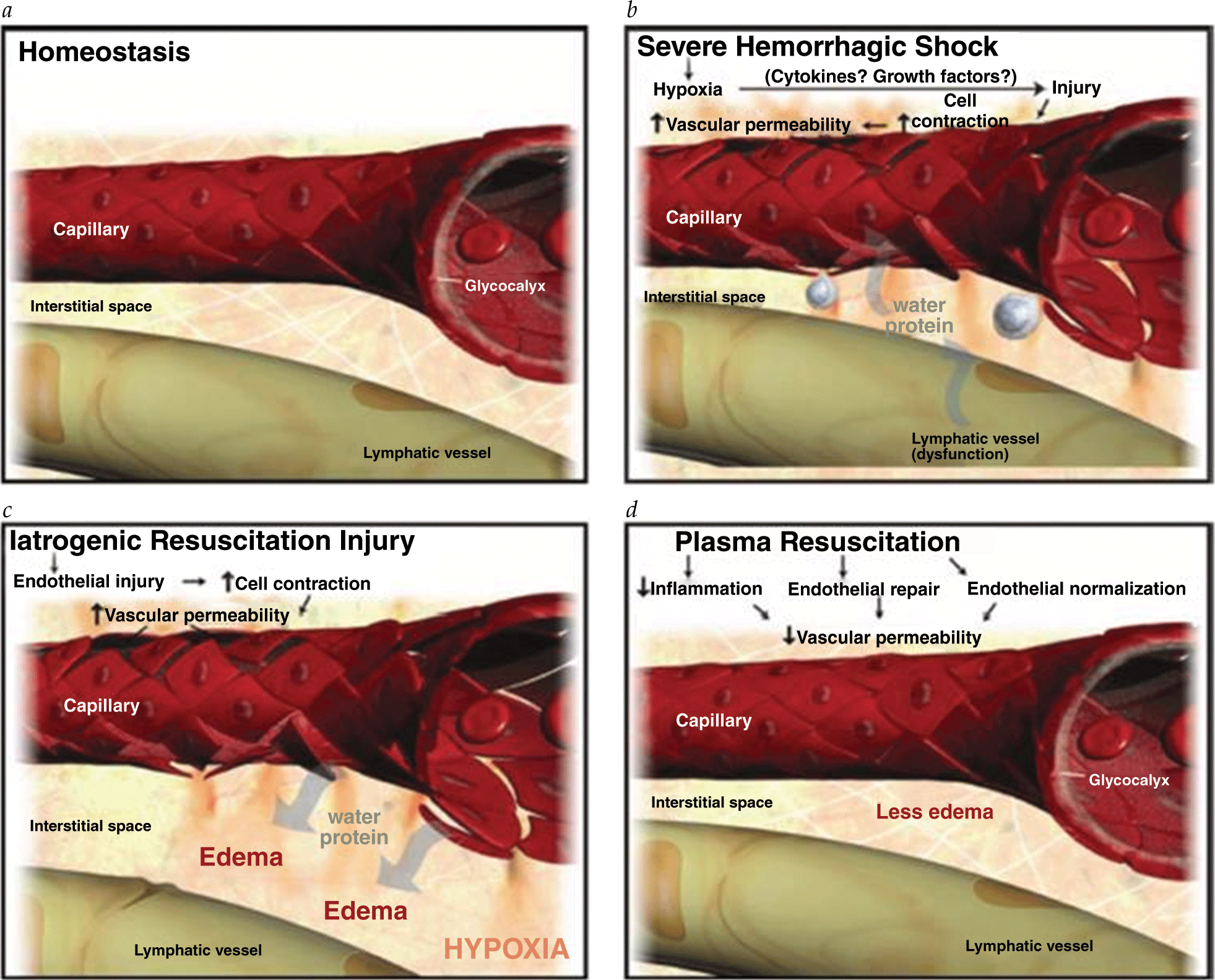
- The Committee on Trauma of the American College of Surgeons (ACS-COT) mandates that high-level trauma centers develop a predefined MTP that can be activated to quickly transfuse rapidly hemorrhaging patients. Early activation of a predefined MTP is associated with more efficient use of blood products (reducing waste) and improved patient outcomes. However, early identification of the bleeding patient remains a challenge.
- Viscoelastic assays such as thromboelastography (TEG) and rotational thromboelastometry (ROTEM) assess the coagulation profile of a whole blood sample. Significantly, different parameters derived from the TEG and ROTEM tracings are related to different components of coagulation, enabling targeted correction of abnormalities.
- Although it seems natural and intuitive to follow the same protocol to treat patients with substantial nontraumatic hemorrhage, there is little scientific evidence to support this practice. Of the few studies investigating optimal blood product ratios of nontraumatic hemorrhage available in the literature, MT was unfortunately defined using the outdated criterion of 10 RBC units or more in 24 hours, which, as we have previously stated, is fraught with survivor bias.


.png)







